Coding for Patient Optimization Work in the Presurgical Period
Author:
Category: Practice Management
Date: May 2021
The AAOS Coding Coverage & Reimbursement Committee in conjunction with the American Association of Hip and Knee Surgeons (AAHKS) Health Policy Council addresses one of the most common coding questions in orthopaedic practices: How should work performed prior to surgery be reported?
To answer this question, we must look to CPT and payer definitions for the global surgical package and consider the evolving nature of the work performed during the presurgical period.
CPT’s definition of the Global Surgical Package
In 2015, the American Medical Association (AMA) revised CPT’s language about the surgical package, and included this discussion of presurgical care:
By their very nature, the services to any patient are variable. The CPT codes that represent a readily identifiable surgical procedure thereby include, on a procedure-by-procedure basis, a variety of services. In defining the specific services “included” in a given CPT surgical code, the following services related to the surgery when furnished by the physician or other qualified health care professional who performs the surgery are included in addition to the operation per se:
- Evaluation and Management (E/M) service(s) subsequent to the decision for surgery on the day before and/or day of surgery (including history and physical
The AMA explained its interpretation of the preoperative element in May 2009.
Question:
Are preoperative visits billable? If so, what code should be used and what is the time frame before surgery to submit this code?
Answer:
If the decision for surgery occurs the day of or before the major procedure and includes the preoperative evaluation and management (E/M) services, then this visit is separately reportable. Modifier 57, Decision for Surgery, is appended to the E/M code to indicate this is the decision-making service, not the history and physical (H&P) alone.
If the surgeon sees the patient and makes a decision for surgery and then the patient returns for a visit where the intent of the visit is the preoperative H&P, and this service occurs in the interval between the decision-making visit and the day of surgery, regardless of when the visit occurs (1 day, 3 days, or 2 weeks) the visit is not separately billable as it is included in the surgical package.
Example: The surgeon sees the patient on March 1 and makes a decision for surgery. Surgery is scheduled for April 1. The patient returns to the office on March 27 for the H&P, consent signing, and to ask and clarify additional questions. The visit on March 27 is not billable, as it is the preoperative H&P visit and is included in the surgical package.
In March 2015, the topic was revisited with the following example:
The Surgeon sees the patient on March 1 and makes a decision for surgery. Surgery is scheduled for April 1. The patient returns to the office on March 27 for the H&P, consent signing, and any needed clarification.
The visit on March 27 is not reported because it is the preoperative H&P visit and is included in the surgical package.
To apply this CPT guidance, one must understand that the work described as “preoperative H&P” entails the required completion of hospital-required paperwork and consent-signing, along with answering patient questions. It does not entail the physician or other qualified healthcare professional (e.g., nurse practitioner, physician assistant) making the final decision for surgery or the work of other supporting services needed to optimize and clear the patient for surgery.
CMS’s Global Surgical Package
The Center for Medicare and Medicaid Services (CMS) publishes its definition of the global surgical package within the Medicare Claims Processing Manual, and it was described in a Medicare Learning Network document titled “Global Surgery Booklet” in September 2018.4 CMS Medicare Administrative Contractors (MACs) have republished this information on their web sites. Medicare’s description of the global surgical package differs slightly from the CPT text, and states:
Medicare includes the following services in the global surgery payment when provided in addition to the surgery:
- Pre-operative visits after the decision is made to operate. For major procedures, this includes preoperative visits the day before the day of surgery. For minor procedures, this includes pre-operative visits the day of surgery.
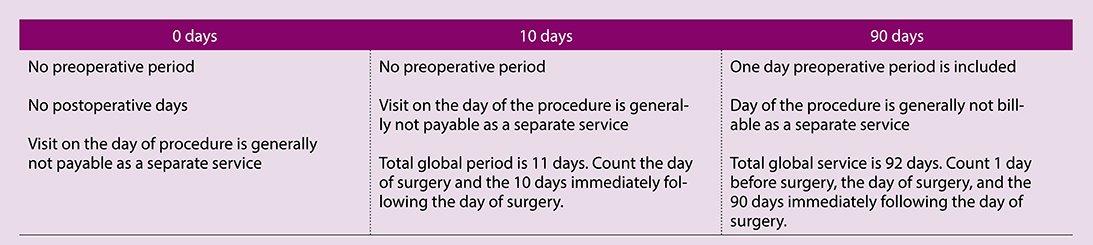
Within that document, Medicare also discusses the fact that surgical codes are assigned as either 0, 10-, or 90-day global codes, and what they include. The information is displayed in Table 1.
Regarding 90-day surgical procedures, the CMS booklet indicates that any preoperative care that does not occur one day prior to surgery would be separately reportable. However, the first sentence of the CMS instruction states that “preoperative visits after the decision is made to operate” are included in the global period, without discussing a time period or the visit intent. At the same time, the second sentence and the itemized lists in the “Global Surgery Booklet” only reference the day prior to the major surgery. The key factor is that the decision to operate is made at the optimization visit (For some common types of presurgical optimization efforts, see the sidebar on page 22).
In 2020, AAOS and AAHKS conducted discussions with the AMA/Specialty Society RVS Update Committee (RUC) and CMS regarding the impact of reductions in relative value units planned in 2021 for total knee arthroplasty (TKA) and total hip arthroplasty (THA). These changes were outlined in the January 2021 edition of AAOS Now (“2021 MPFS: What It Means for Your THA and TKA Reimbursement”). During those discussions, it became clear that CMS and the RUC consider the global period for a 90-day global code as starting the 24 hours prior to surgery.
Current delivery of surgical care
Since 2009, many changes have occurred in the delivery of surgical care. A quick patient history and physical exam in the office the day before surgery is a thing of the past. Bundled payments and presurgical optimization of the patient have become standard for many procedures. With these changes in care, much of the work to optimize patients for surgery and the postoperative recovery period have moved into the presurgical period.
These shifts have resulted in better outcomes for patients and dramatic cost savings for insurance carriers. There has been a marked decrease in the need for patients to go to rehabilitation units or skilled nursing facilities. The number of post-procedure days in the hospital has also decreased, and the rate of infections in total joints has declined due to better presurgical screening. All these improvements in care are accomplished through effective presurgical optimization of the patient by providers between the point when surgery is first considered and the day of the procedure.
None of these assessment activities are valued in the presurgical work of musculoskeletal surgery CPT codes. We recommend CPT codes that can be used to describe presurgical optimization services. Payment for use of these CPT codes will vary according to payer policies.
CPT codes which could describe presurgical optimization services
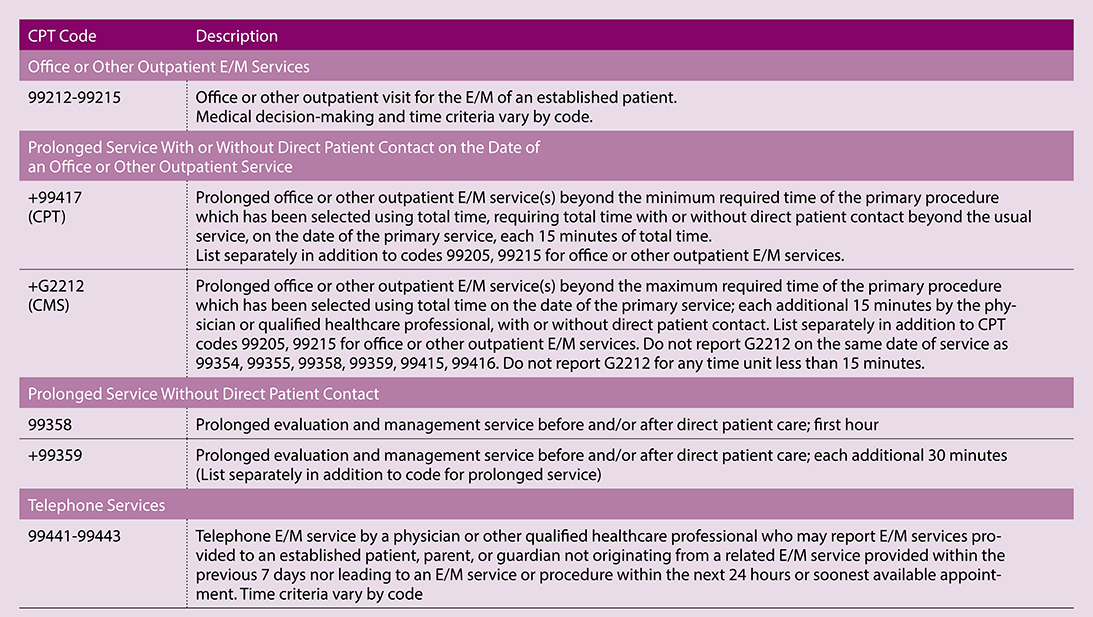
AAOS and AAHKS extensively reviewed the current edition of the CPT manual, specifically the Evaluation & Management Services Guidelines as well as codes within the Office or Other Outpatient Services, Prolonged Services, and Telephone Services. The guidelines for each are outlined below followed by the appropriate reportable codes (Table 2).
Office or Other Outpatient E/M Services
Guidelines for assigning medical decision making (MDM) credit under the current E/M guidelines for office services may limit the level of service when using MDM for selecting codes for an optimization visit. For example, if a provider using MDM to select a level of service takes credit for consideration of major surgery under the Risk element during an initial evaluation, it is not clear if the same credit can be assigned when the decision for surgery is finalized. Using Time to determine the level of service for an optimization visit is reasonable and supported.
Prolonged Service With or Without Direct Patient Contact on the Date of an Office or Other Outpatient Service CPT instructions allow prolonged services time on the date of the E/M encounter to be counted after the minimum range of the 99205 or 99215 service is met, but CMS requires that prolonged time is reported after the maximum required time for the primary service.
Example: If a provider spends 55–69 minutes (including face-to-face and non–face-to-face services) on the date of an optimization visit, code +99417 could be reported in addition to code 99215. For CMS, 70–84 minutes would be required in order to report +G2212 in addition to 99215.
Prolonged service without direct patient contact:
These codes include time that physicians or other qualified healthcare professionals (QHPs) spent providing indirect contact services in relation to patient management where face-to-face services have or will occur on a different date.
CPT instructions state that codes 99358 and 99359 cannot be used during the same session as codes 99202–99215, but the September 2020 CPT Assistant stated that these codes can be reported for care related to office or other outpatient services that occurred on a different date.
However, in the 2021 Medicare Physician Fee Schedule, CMS disagreed and stated they will not allow payment for codes 99358/99359 in relation to codes 99202–99215, even for services on a different date. Other payer rules may vary.
Time spent providing prolonged services applies to a given date, even when time is not continuous. The calculation of time would not include cumulative services provided over multiple dates. The CPT coding rule for reporting time-based codes applies (e.g., a unit of time is attained when the midpoint has passed).
Example: A provider assessing a patient for surgery documents spends 35 minutes reviewing consultation reports from the internist and endocrinologist, along with laboratory and imaging results and formulating a plan for surgery. The provider would report code 99358, because greater than the midpoint requirement of one hour was achieved.
Telephone Services
Payer policies for telephone E/M services may vary, particularly during a public health emergency.
Final thoughts
Many of the steps now required for presurgical decision making and patient optimization are not represented by the term “history and physical” and are not included in the definitions of the global surgical package. With changes in the delivery of care, it is reasonable and appropriate for physicians and QHPs to report optimization services using existing CPT codes in the presurgical period.
References
- Current Procedural Terminology, 2021
- CPT Assistant, “Coding Clarification (May 2009).” Available at https://www.findacode.com/newsletters/ama-cpt-assistant/coding-clarification-2009-5.html.
- CPT Assistant, “Your Quick Guide to the Global Surgical Package.” Available at https://www.aapc.com/blog/46373-your-quick-guide-to-the-global-surgical-package/.
- CMS Medicare Learning Network: Global Surgery Booklet, September 2018. Accessed April 13, 2021. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/GloballSurgery-ICN907166.pdf.
- Bernstein DN, Liu TC, Winegar AL, et al: Evaluation of a Preoperative Optimization Protocol for Primary Hip and Knee Arthroplasty Patients. J Arthroplasty 2018(33):3642-48.
- Grosso MJ, Courtney PM, Kerr JM, et al: Surgeons’ Pre-Operative Work Burden Has Increased Prior to Total Joint Arthroplasty: A Survey of AAHKS Members. J Arthroplasty 2020:35(6):1453-57.
- Iorio R, Clair AJ, Inneh IA, et al: Early Results of Medicare’s Bundled Payment Initiative for a 90-Day Total Joint Arthroplasty Episode of Care. J Arthroplasty 2016:31(2):343-50.
- Dundon JM, Bosco J, Slover J, et al: Improvements in Total Joint Replacement Quality Metrics: Year one Versus Year Three of the Bundled Payments for Care Improvement Initiative. J Bone Joint Surg Am 2016;98(23): 1949-53.
- Navathe AS, Troxel AB, Liao JB, et al: Cost of Joint Replacement Using Bundled Payment Models. JAMA Intern Med 2017;177(2):214-22.
- Siddiqi A, White PB, Mistry JB, et al: Effect of Bundled Payments and Health Care Reform as Alternative Payment Models in Total Joint Arthroplasty: A Clinical Review. J Arthroplasty 2017;32(8):2590-7.
- Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R: Total knee arthroplasty: improving outcomes with a multidisciplinary approach. J Multidiscip Healthc 2018;11:63-73.
- Barnett ML, Wilcock A, McWilliams JM, et al: Two year Evaluation of Mandatory Bundled Payments for Joint Replacement. N Engl J Med 2019;380(6):252-62.
- Wasterlain AS, Courtney PM, Yayac MF, et al: Quantifying the Perioperative Work Associated with Total Hip and Knee Arthroplasty: The Burden Has Increased With Contemporary Care Pathways. J Arthroplasty 2019;34(11):2528-31.
- Kheir M, Rondon AJ, Bonaddio V, et al: Perioperative Telephone Encounters Should Be Included in the Relative Value Scale Update Committee Review of Time Spent on Total Hip and Knee Arthroplasty. J Arthroplasty 2019;34(8):1563-9.
- Krueger CA, Kerr JM, Bolognesi MP, et al: The Removal of Total Hip and Total Knee Arthroplasty from the Inpatient Only List Increases the Administrative Burden of Surgeons and Continues to Cause Confusion. J Arthroplasty 2020;35(10):2772-8.
- Krueger CA, Austin MS, Levicoff EA, et al: Substantial Preoperative Work Is Unaccounted for in Total Hip and Knee Arthroplasty. J Arthroplasty 2020:35(9): 2318-22. https://www.arthroplastyjournal.org/article/S0883-5403(20)30454-X/fulltext
- Rondon AJ, Phillips JLH, Fillingham YA, et al: Bundled Payments Are Effective in Reducing Costs Following Bilateral Total Joint Arthroplasty. J Arthroplasty 2019;34(7):1317-21.
Common coding scenarios
The three detailed scenarios (see the accompanying sidebars) describe common examples of presurgical optimization work which are not included in surgical CPT code definitions or CMS-assigned relative values.
Scenario 1: Provider (MD, DO, PA, NP) Face-to-Face Decision for Surgery
A 70-year-old woman returns to the office with severe knee arthritis refractory to non-operative measures. Her physical exam and radiographs indicate a total knee replacement would be her best option. She is being considered for unilateral knee replacement (27447, 90-day global). Her comorbidities include hypertension, unstable diabetes, and atrial fibrillation which requires an anticoagulant. She is sent to see her internist, endocrinologist, and cardiologist for preoperative clearance consultations. The patient returns to the office and the provider reviews all the records and gets up-to-date laboratory values. If the findings from the clearance consultations and laboratory testing indicate the patient is able to proceed with surgery, the provider then proposes surgery as a definitive recommendation. The provider explains the specifics of the proposed procedure and initiates other presurgical optimization steps.
Analysis: Both of these visits are billable as an established patient office visit E/M code, with the level of the visit determined by the documentation (99212-99215, +99417, +G2212). The global period for her surgery will start the day before the operation. When the surgeon sees the patient the day of surgery prior to the operation that visit is not billable. This is because the preoperative time of that visit has already been valued in the 90-day global code (CPT 27447) as part of the pre-time package.
Scenario 2: Provider Non-Face-to-Face
A patient seen two weeks ago for whom surgery was one management option considered, has all his records (recent consultations, imaging, and labs) sent to the office for consideration of definitive surgical management. A review of the records by the provider reveals that the patient is healthy enough and therefore the patient is offered surgery as definitive surgical management.
Analysis: The provider may report a code or codes for Prolonged Service Without Direct Patient Contact (99358, +99359), depending upon the amount of time spent and documented. At least 30 minutes is required to support code 99358.
Scenario 3: Provider Telephone Call to Discuss Preoperative Clearance
A similar patient to scenario 2 who lives a distance away from the office requests a phone visit with the provider to discuss the outcome of their presurgical clearance. The provider goes over the consultations and lab results with the patient and determines that the patient is an appropriate candidate for surgery. They then discuss the perioperative plan and discharge management arrangements. The call takes 30 minutes.
Analysis: The provider may report a code or codes for Telephone Services (99441-99443), depending upon the amount of time spent and documented. Keep in mind, the CPT definition includes limitations for telephone services originating from or related to a visit within the previous seven days and leading to an E/M service or procedure within the next 24 hours or soonest available appointment.