Outpatient Total Hip Arthroplasty Trends Continue to Shift
Author: Brooks Martino, BA;Drake G. LeBrun, MD;Michael P. Ast, MD, FAAOS
Category: Clinical;Hip & Knee
Date: Jul 2021
Total hip arthroplasty (THA) has seen a shift in recent decades toward shorter inpatient stays, including outpatient procedures in selected patients. This shift has been driven in part by advances in perioperative care and surgical techniques, as well as an increasing focus on reducing costs per episode of care. It is estimated that, by 2026, over half of all hip and knee arthroplasty procedures will be performed on an outpatient basis.
Outpatient THA has been shown to benefit both patients and the healthcare system, with comparable complication rates, outcomes, and patient satisfaction relative to traditional inpatient THA. Advancements in multiple areas, such as patient selection, multimodal anesthesia, and multidisciplinary care pathways, have significantly bolstered our ability to successfully discharge patients on the day of surgery.
However, multiple challenges remain. Algorithms attempting to identify patients at risk for failed same-day discharge are complicated and imperfect. Furthermore, addressing postoperative complications post-discharge and coordinating unplanned admissions can be a logistically taxing task for the hospital, surgeon, and surgical office staff.
This article reviews the current state of outpatient THA compared to traditional inpatient THA, factors contributing to successful outpatient THA, the persistent challenges associated with outpatient THA, and directions for expansion and improvement.
Inpatient versus outpatient THA
Over the past two decades, numerous studies have compared outcomes of outpatient and inpatient THA. These studies have largely reported similar or better complication and readmission rates with outpatient THA. Most studies also found that patients experienced excellent short-term physical function and pain scores after outpatient THA, as well as high levels of satisfaction, with 96–97 percent of patients satisfied with the decision to undergo outpatient THA.
However, the authors of these studies acknowledge that selection bias significantly impacts these findings. Patients undergoing outpatient THA are generally younger and healthier to meet criteria for outpatient surgery. Not surprisingly, patients at increased risk for complications and readmissions after outpatient THA are generally older with more comorbidities.
Given an increasing national focus on value-base care, potential cost savings is another area of study related to outpatient THA. Studies comparing costs after outpatient versus inpatient THA have found moderate cost reductions with outpatient THA, but it is important to note that these economic savings can only be preserved if complication and readmission rates following outpatient THA do not outpace corresponding rates for inpatient procedures.
Keys to success
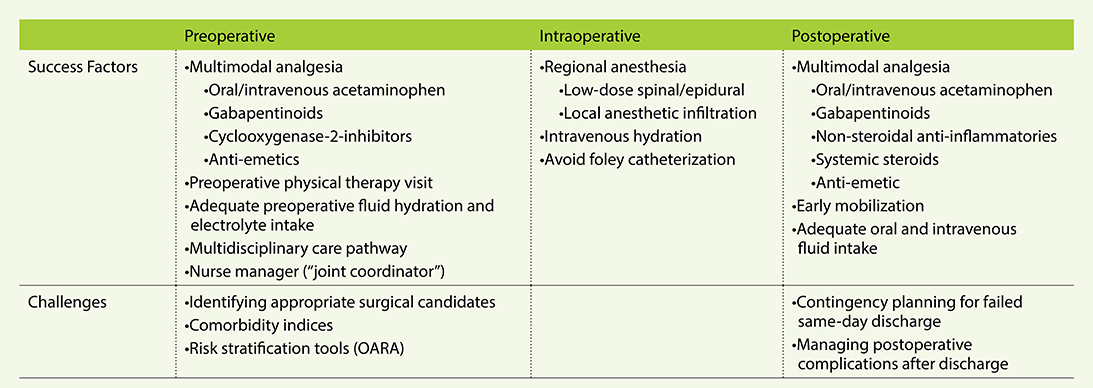
Successful outpatient THA has been made possible due to advances in multiple realms, including multimodal anesthesia, blood and fluid management, early mobilization, and multidisciplinary care pathways (Table 1).
Multimodal anesthesia protocols use anesthetic agents with complementary mechanisms of action during the preoperative, intraoperative, and postoperative phases of care. Preoperative protocols may include the use of a combination of oral or intravenous acetaminophen, gabapentinoids, cyclooxygenase-2-inhibitors (e.g., celecoxib), and antiemetics (e.g., ondansetron, metoclopramide, and/or scopolamine).
Preoperative opioids can also be used; however, the use of perioperative opioids must be weighed with possible side effects related to nausea and impaired mobilization. Intraoperative analgesia generally relies on low-dose spinal or epidural anesthesia or general anesthesia in conjunction with local anesthetic infiltration of the anterior hip capsule, periarticular soft tissues, and subcutaneous tissues. These local infiltrates can also be supplemented by plain or liposomal bupivacaine, epinephrine, antibiotics, and steroids.
Postoperatively, given the importance of early mobilization in an outpatient setting, a multimodal strategy is critical to address pain and nausea while permitting early ambulation. This can be done via a combination of acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), gabapentinoids, antiemetics, and systemic steroids. Opioids should be used sparingly, and only when necessary, so as not to interfere with mobilization or increase postoperative nausea.
Blood and fluid management throughout the perioperative period is crucial because nausea, dizziness, and urinary retention are among the most common reasons for failed same-day discharge. Preoperative and postoperative oral fluid intake, in addition to adequate intravenous hydration and avoiding Foley catheterization, when possible, can aid in this regard by ensuring adequate hydration and easier voiding postoperatively.
Another chief tenet of outpatient arthroplasty is safe, early mobilization upon return of full motor function after regional anesthesia. The goal of postoperative protocols in an outpatient setting is to ensure a safe return home once the patient can meet certain discharge readiness criteria, such as independence with transfers, ascending and descending stairs, and ambulating a certain distance with or without assistance.
Importantly, some physicians recommend starting physical therapy prior to surgery with an initial visit to set expectations, provide a foundational understanding of key exercises, outline postoperative restrictions, and define specific therapy goals based on the patient’s baseline function.
Lastly, multidisciplinary care pathways incorporating the surgical, nursing, anesthesia, and physical therapy teams have been a critical contributor to the growth of outpatient arthroplasty. These teams can jointly evaluate the safety and appropriateness for outpatient arthroplasty on a patient-by-patient basis, set up a safe discharge plan, and align expectations. A nurse manager or “joint coordinator” may be helpful by serving as a point person to coordinate multiple care pathways.
Remaining challenges
Despite the many advances in perioperative care that have enabled the growth of outpatient THA, some challenges persist.
Identifying patients who are appropriate candidates for outpatient THA is still an imperfect science. To address the shortcomings of comorbidity indices, Meneghini et al. developed a novel risk stratification tool called the Outpatient Arthroplasty Risk Assessment Score (OARA) to measure the prevalence, severity, and control of various conditions within nine different medical comorbidity realms. Although the OARA may outperform simple comorbidity indices as a risk stratification tool, medical comorbidities may not provide sufficient information on other relevant factors such as social support, home resources, and dependent physical function.
Another critical challenge is in the management of patients who fail same-day discharge, particularly in an ambulatory surgery center (ASC). Compared to hospitals, ASCs are unique in that they do not have the capacity to admit patients overnight should they need additional care and observation following THA. As such, ASCs must prepare contingency plans for transfers and admissions to nearby hospitals that can support overnight stays. The logistical coordination on part of the ASC, hospital, surgeon, and office staff can be significant.
Similarly, a quicker timeline for discharge after THA does not translate to a quicker timeline for complications or postoperative recovery. In contrast to inpatient THA, outpatient THA yields a more dynamic and less predictable postoperative recovery for patients, as they are subject to the variable limitations of being in their own home with their own support system instead of the more controlled environment of the hospital. This can lead to more variability in recovery with fewer “eyes” on the patient to monitor for complications, particularly within the first 24 hours.
Future directions
In 2021, ambulatory THA appears to be a safe, effective, and potentially lower-cost alternative to traditional inpatient THA for selected patients. However, as ambulatory THA continues to grow in popularity, areas for growth and improvement remain. Patient selection protocols are still evolving, and future research should be aimed at developing, refining, and validating existing and new selection criteria.
Furthermore, much of the current literature is based on outpatient THA performed in a hospital as opposed to an ASC, and understanding the differences in these two settings, with a special focus on coordinating unplanned admissions from an ASC, is merited. In addition, with numerous studies exploring reasons for failed same-day discharge, the field should continue to hone perioperative measures aimed to overcome the most common reasons patients fail same-day discharge such as pain, nausea, urinary retention, and hypotension.
Brooks Martino, BS, is a fourth-year medical student at Weill Cornell Medical College.
Drake G. LeBrun, MD, MPH, is a fourth-year orthopaedic resident at Hospital for Special Surgery.
Michael P. Ast, MD, FAAOS, is an assistant professor of Orthopaedic Surgery at Weill Cornell Medical College and a Joint Replacement Surgeon at Hospital for Special Surger. He is a member of the Knee Reconstruction Evaluation Committee, an AAOS webinar moderator, and a member of the faculty for the AAOS Board Preparation and Review Course and the AAOS Outpatient and Rapid Recovery in Total Joint Replacement.
References
- Foote J, Panchoo K, Blair P, Bannister G: Length of stay following primary total hip replacement. Ann R Coll Surg Engl 2009;91(6):500–4.
- Petersen PB, Jørgensen CC, Kehlet H: Temporal trends in length of stay and readmissions after fast-track hip and knee arthroplasty. Dan Med J 2019;66(7):1–4.
- Bert JM, Hooper J, Moen S: Outpatient Total Joint Arthroplasty. Curr Rev Musculoskelet Med 2017;10(4):567–74.
- Jaibaji M, Volpin A, Haddad FS, Konan S: Is Outpatient Arthroplasty Safe? A Systematic Review. J Arthroplasty 2020;35(7):1941-1949.
- Courtney PM, Rozell JC, Melnic CM, Lee GC: Who Should Not Undergo Short Stay Hip and Knee Arthroplasty? Risk Factors Associated With Major Medical Complications Following Primary Total Joint Arthroplasty. J Arthroplasty 2015;30(9):1–4.
- Sher A, Keswani A, Yao D, et al: Predictors of Same-Day Discharge in Primary Total Joint Arthroplasty Patients and Risk Factors for Post-Discharge Complications. J Arthroplasty 2017;32(9):S150-S156.e1.
- Goyal N, Chen AF, Padgett SE, et al: Otto Aufranc Award: A Multicenter, Randomized Study of Outpatient versus Inpatient Total Hip Arthroplasty. Clin Orthop Relat Res 2017;475(2):364–72.
- Dorr L, Thomas D, Zhu J, et al: Outpatient Total Hip Arthroplasty. J Arthroplasty 2010;25(4):501–6.
- Pansard E, Klouche S, Bauer T, et al: Can primary total hip arthroplasty be performed in an outpatient setting? Prospective feasibility and safety study in 321 patients in a day-surgery unit. Orthop Traumatol Surg Res 2020;106(3):551–5.
- Hoeffel D, Kelly B, Myers F. Patient Reported Outcomes: Inpatient vs. Outpatient Total Hip Arthroplasty. Orthop Proc 2018;98-B(Supp 8).
- Aynardi M, Post Z, Ong A, et al: Outpatient Surgery as a Means of Cost Reduction in Total Hip Arthroplasty: A Case-Control Study. HSS J 2014;10(3):252–5.
- Bertin KC. Minimally invasive outpatient total hip arthroplasty: A financial analysis. Clin Orthop Relat Res 2005;(435):154–63.
- Nassar I, Fahey J, Mitchell D. Rapid recovery following hip and knee arthroplasty using local infiltration analgesia: length of stay, rehabilitation protocol and cost savings. ANZ J Surg 2020;90(3):355–9.
- Shah RP, Karas V, Berger RA: Rapid discharge and outpatient total joint arthroplasty introduce a burden of care to the surgeon. J Arthroplasty 2019;34(7):1307–11.
- Meneghini RM, Ziemba-Davis M, Ishmael MK, et al: Safe Selection of Outpatient Joint Arthroplasty Patients With Medical Risk Stratification: the “Outpatient Arthroplasty Risk Assessment Score.” J Arthroplasty 2017;32(8):2325–31.
- Ziemba-Davis M, Caccavallo P, Meneghini RM: Outpatient Joint Arthroplasty—Patient Selection: Update on the Outpatient Arthroplasty Risk Assessment Score. J Arthroplasty 2019;34(7):S40–3.
- Bovonratwet P, Shen TS, Ast MP, et al: Reasons and Risk Factors for 30-Day Readmission After Outpatient Total Knee Arthroplasty: A Review of 3015 Cases. J Arthroplasty 2020;35(9):2451–7.
- Sah A: Considerations for Office and Staff Protocols for Outpatient Joint Replacement. J Arthroplasty 2019;34(7):S44–5.