Biceps Tenotomy and Tenodesis Can Be Addressed by a Variety of Surgical Approaches
Author: Miriam D. Weisberg, MD;Alan M. Reznik, MD, MBA, FAAOS
Category: Clinical
Date: Mar 2022
Editor’s note: This article is the second in a two-part series on the controversies in treatment for symptomatic long head of the biceps. This article examines the details of surgical treatments, complications, as well as the pros and cons of the common approaches.
As explored in the February issue of AAOS Now (“Put the Flex back in Flexing: The Best Treatment of Biceps Tendonitis”), the differing etiologies of tendinopathy or injury to the long head of the biceps tendon (LHBT) lead to a variety of patient presentations.
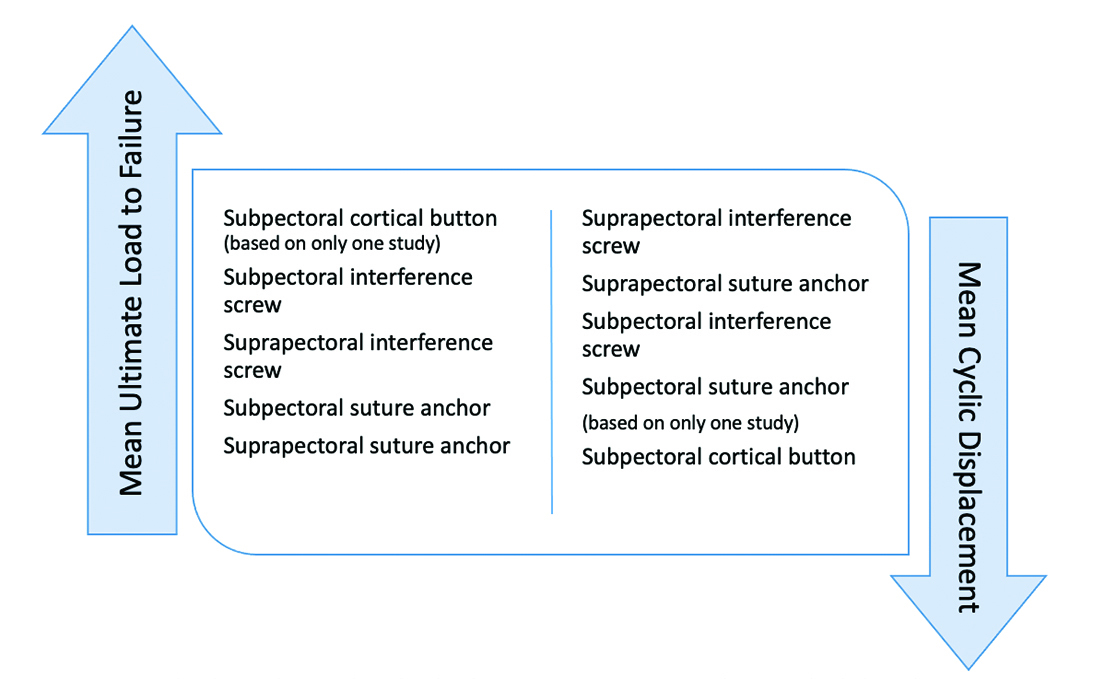
Regardless of the mechanism, treatment is tailored to patient-specific demands and expectations. Fig. 1 shows the relative mechanical fixation properties reported in the literature.
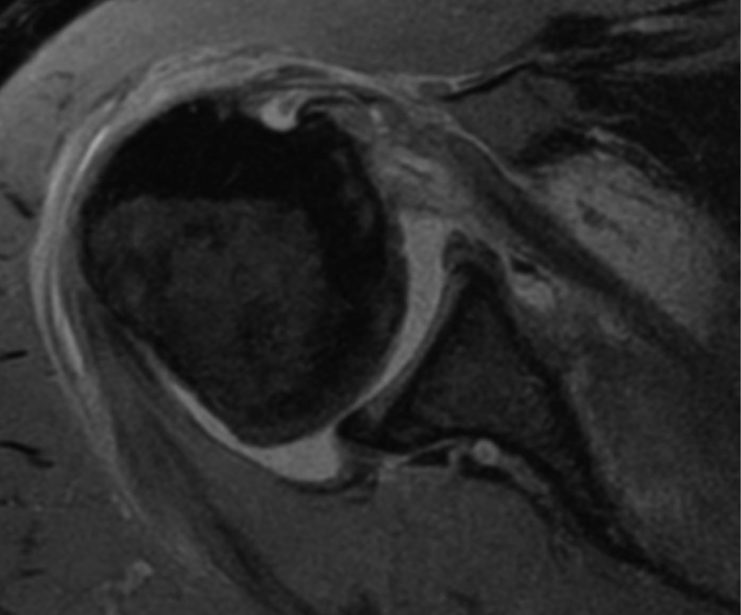
Post-traumatic or recalcitrant biceps pain with positive clinical tests should be imaged to localize pathology along the biceps tendon, as well as any coexisting pathology (Fig. 2). Indications for surgery include partial-thickness tear of at least 25 to 50 percent, medial subluxation, instability with a subscapularis tear, and/or biceps pulley tear. In addition, unstable superior labral tear anterior to posterior (SLAP) lesions, including an unstable, symptomatic type II SLAP tear and the subset of unstable bicep anchor lesions, are associated with a variety of more complex SLAP tears in patients older than 50 years or patients in whom symptoms failed to improve after a prior SLAP repair.
Arthroscopic assessment
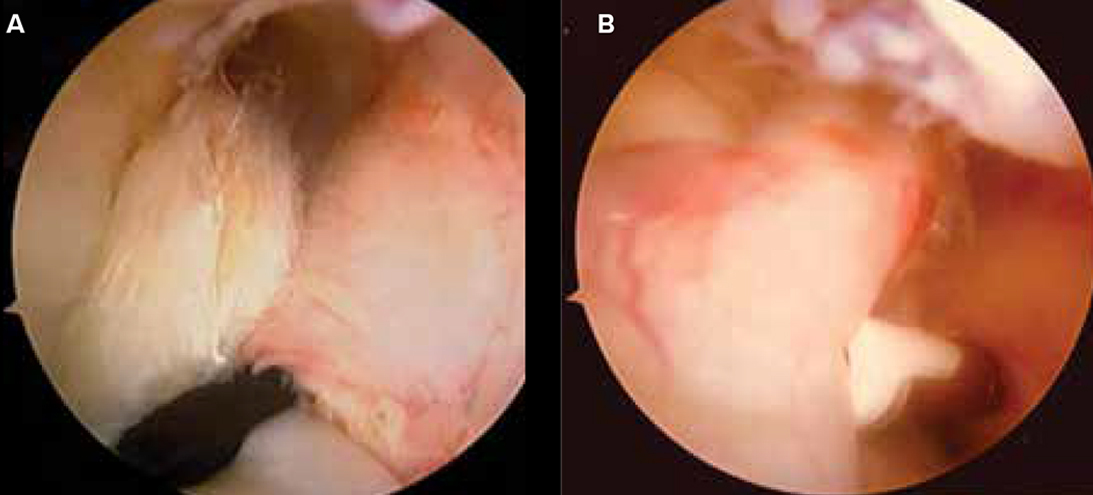
It is important to visualize the tendon to assess for hypertrophy or induration, which may best be seen prior to insufflating the joint. Instability at the edge of the subscapularis and the biceps’ proximal anchor (i.e., SLAP lesion) is assessed by attempting to subluxate the tendon with a probe. The rotator cuff is checked for tears at the superior edge of the subscapularis (the “comma”) and near the “biceps exit” from the glenohumeral joint (Fig. 3). The tendon must also be pulled into the glenohumeral joint to visualize the portion lying just past the biceps exit, understanding this area is particularly susceptible to tendon pathology and partial tearing. Evaluation including these key elements helps determine the best treatment for biceps pathology.
Tenotomy
The tendon is cut as close to its origin as possible while preserving the superior labral ring. Tendons can fail to retract due to scarring within the bicipital groove. This remaining intra-articular tendon can cause residual pain. Patients should be aware of a possible postoperative Popeye deformity and potential cramping in the upper arm with repetitive use. Treatment of coexisting pathology, such as rotator cuff and SLAP tears, is required to ensure optimal results.
Tenodesis
Tenodesis can be performed proximally, where the tendon remains in the groove, or distally, where the tendon is removed from the groove and transposed. Tenodesis can be performed with open (subpectoral) or arthroscopic (suprapectoral, all-arthroscopic, and arthroscopic-assisted) techniques. Arthroscopic suprapectoral and open subpectoral tenodesis for isolated unstable SLAP/biceps lesions have shown equivalent patient-reported outcome scores in both function and strength at two years postoperatively. The most complete debridement is carried out with a combined approach.
Following arthroscopic evaluation, a spinal needle can be used to hold the tendon while a tenotomy is performed. The ideal site of arthroscopic tenodesis is 1 cm distal to the superior aspect of the bicipital groove. The tendon is then secured to the biceps sling (i.e., percutaneous intra-articular trans-tendon technique), or the bone is prepared arthroscopically and secured with a suture anchor, cortical button, or interference screw. Suprapectoral drill holes create less of a stress riser and, hence, a lower risk of fracture than distal cortical holes.
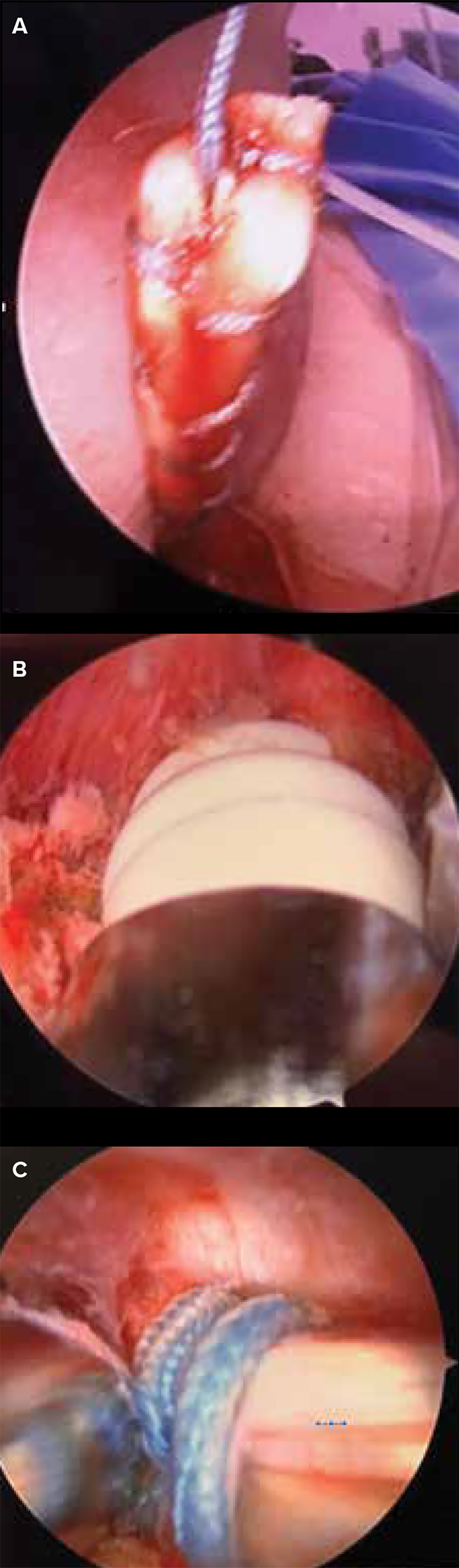
In an open approach, a subpectoral incision is made. The tendon is located and presented through the wound. A locking stitch is used to secure the tendon from 15 mm proximal of the musculotendinous junction. Excess diseased tendon is excised. The humeral shaft is prepared within the bicipital groove 1 cm proximal to the pectoralis insertion (Fig. 4). One technique is to create a keyhole-shaped hole in which a knot of tendon is interposed. Although this method does not require any special equipment and allows early range of motion, it does so by creating a large cortical defect and has a failure rate of up to 20 percent. Similarly, bone tunnels may create a large stress riser and place additional stress on the tendon when it is passed around a “killer turn” within the groove. Healing rates between bone tunnels and cortical bone are similar, making the additional risk associated with utilizing bone tunnels unnecessary.
Alternatively, the tendon can be secured with an inlay (interference screw) or onlay (unicortical button or suture anchor). With an interference screw, a hole is reamed, the tendon is interposed in the hole, and the tendon is secured with a screw. This technique has been shown to be biomechanically stronger than alternative fixation methods but has no significant clinical difference in outcome measures. Inlay approaches can also cause a potential stress riser and lead to fracture.
SLAP and return to sports
The traditional mantra for surgical decisions was “under 40 years old, repair; over 40 years old, tenodesis.” Now, the indications are more patient-specific. The first-line surgical approach in management of most young individuals with acute trauma or type IV SLAP tears is repair and preservation of native anatomy. Interestingly, as new evidence continues to emerge, this approach may also evolve.In patients with LHBT pathology with a SLAP tear, the return to play in competitive athletes has been shown to be as high as 87 percent with tenodesis, compared with 20 percent after SLAP repair alone. Notably, 60 percent of patients reported that they were unsatisfied following SLAP repair alone. Newer studies have shown positive outcomes with tenodesis even in overhead-throwing athletes younger than 25 years old. Note that the studies were not limited to type IV SLAP tears.
Complications
Popeye deformity can occur after tenotomy, and there is still a small risk of the deformity following tenodesis, regardless of approach or fixation method. Reported Popeye deformity ranges from 3 percent to 70 percent. A recent randomized clinical trial showed a 3.5-fold higher rate of Popeye deformity following tenotomy when compared to tenodesis.
Tenotomy below the pectoralis tendon (subpectoral) as well as all-arthroscopic proximal tenotomy, both leaving tendon in the grove and without complete debridement of the groove, risk pain generation from residual diseased tissue within the groove. A recent study reported a higher rate of cramping following tenotomy compared with tenodesis (20 percent versus 8 percent). Thirty-eight percent of patients who underwent tenotomy reported fatigue and discomfort after repetitive use.
Other studies demonstrate that open subpectoral tenodesis more reliably restores anatomic length and prevents overtightening. Arthroscopic tenodesis was more likely than open tenodesis to over-tension the biceps tendon by shortening the tendon. Failure of fixation was more frequent and occurred at a lower force in arthroscopic fixation (seven of nine cadavers) compared to open tenodesis (one of nine cadavers). Tenodesis with suture anchors has higher rates of persistent pain compared to the use of interference screws.
Complications with open subpectoral biceps tenodesis are as low as 2 percent but include failure of fixation with subsequent deformity, continued pain, musculocutaneous neuropathy, reflex sympathetic dystrophy (RSD), and infection.
Causalgia (RSD and complex regional pain syndrome) with injury to the musculocutaneous nerve is a risk with subpectoral tenodesis. Neuropraxia during an open procedure may be due to retraction given the proximity to the brachial plexus. The senior author has reported one case of nerve entrapment secondary to an error in technique. The patient developed causalgia, most likely due to the short head of the biceps becoming entrapped within the tenodesed tendon. The patient subsequently underwent a tenotomy and nerve decompression with resolution of symptoms.
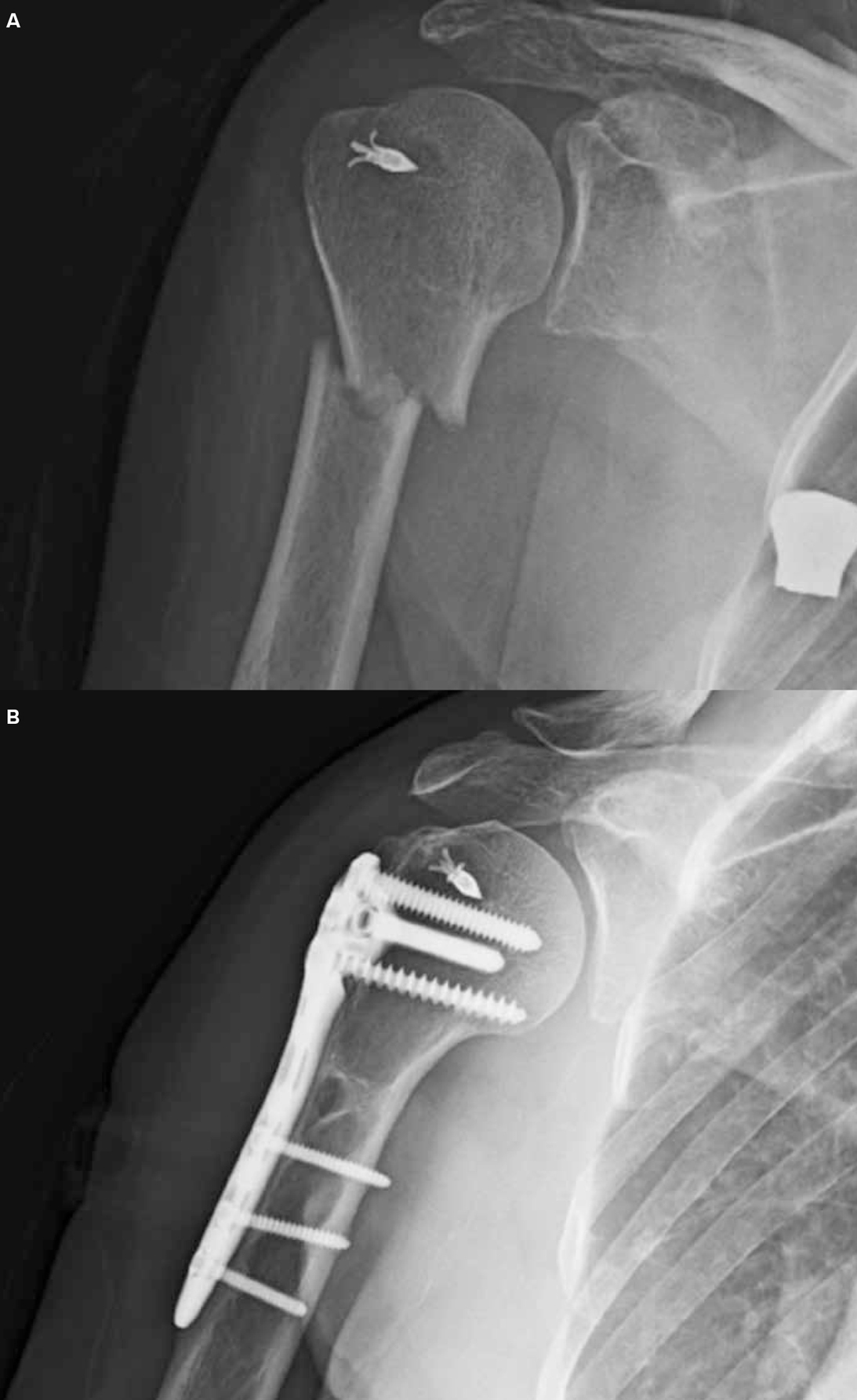
A bone tunnel or bone window for fixation can be a stress riser, and torsional fractures can occur. Studies have demonstrated that less-than-ideal positioning (eccentric-lateral) of the bone window increases torsional stress on the humeral shaft, predisposing the patient to postoperative humeral shaft fracture. A recent review cited a 1.4 percent rate of postoperative humeral shaft fracture (Fig. 5, page 9).
Stiffness, over-tightening, and re-rupture after repair are additional complications of tenodesis. The senior author recounted one case of re-rupture
following a mechanical fall in a thin patient (BMI, 18). Implant failure occurred just below the subpectoral tenodesis site using an interference screw method. A revision with soft-tissue anchors yielded a good outcome. Low BMI, often associated with delayed healing and osteoporosis, and overtightening are risk factors in these types of cases. Studies have demonstrated that the most common site of failure is at the tendon-bone interface.
For biceps pain, patient selection, underlying pathology, and operative technique play a role in clinical outcomes. Although still controversial, the choice between tenotomy and tenodesis is coming into focus. Functional outcomes vary with technique. When orthopaedic surgeons consider risks and expectations, they can improve patient satisfaction.
Miriam D. Weisberg, MD, is an orthopaedic surgery resident at Maimonides Medical Center in Brooklyn, N.Y.
Alan M. Reznik, MD, MBA, FAAOS, is chief medical officer of Connecticut Orthopaedics, an assistant professor of orthopaedics at Yale University School of Medicine, and associate professor of surgery at the Quinnipiac University Frank Netter School of Medicine.
References
- Nho SJ, Strauss EJ, Lenart BA, Provencher MT, Mazzocca AD, Verma NN, Romeo AA: Long head of the biceps tendinopathy: diagnosis and management. J Am Acad Orthop Surg. 2010;18(11):645-56.
- Gill TJ, McIrvin E, Mair SD, Hawkins RJ: Results of biceps tenotomy for treatment of pathology of the long head of the biceps brachii. J Shoulder Elbow Surg. 2001;10(3):247-9.
- Aflatooni JO, Meeks BD, Froehle AW, Bonner KF: Biceps tenotomy versus tenodesis: patient-reported outcomes and satisfaction. J Orthop Surg Res. 2020; 15(1):56.
- Eliasberg CD, Maas JT, O’Brien SJ, Taylor SA: Anatomy of the biceps tendon: from origin to insertion. In: Romeo AA, Erickson BJ, Griffin JW (Eds.), The Management of Biceps Pathology: A Clinical Guide from the Shoulder to the Elbow. Springer, 2021, pp 3-14.
- Kelly AM, Drakos MC, Fealy S, Taylor SA, O’Brien SJ: Arthroscopic release of the long head of the biceps tendon: functional outcome and clinical results. Am J Sports Med 2005;33(2):208-13.
- Virk MS, Cole BJ: Proximal biceps tendon and rotator cuff tears. Clin Sports Med. 2016;35(1):153-61.
- Lee HJ, Jeong JY, Kim CK, Kim YS: Surgical treatment of lesions of the long head of the biceps brachii tendon with rotator cuff tear: a prospective randomized clinical trial comparing the clinical results of tenotomy and tenodesis. J Shoulder Elbow Surg. 2016; 25(7):1107-14.
- Werner BC, Evans CL, Holzgrefe RE, et al: Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of minimum 2-year clinical outcomes. Am J Sports Med. 2014;42(11):2583-90.
- Sanders BS, Warner JJ, Pennington S, Lavery KP: Biceps tendon tenodesis: Success with proximal versus distal fixation. 74th Annual Meeting Proceedings. Rosemont, IL: American Academy of Orthopaedic Surgeons, 2007, p 572.
- Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, Bicknell R: Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929-36.
- Griffin JW, Cvetanovich GL, Kim J, et al: Biceps tenodesis is a viable option for management of proximal biceps injuries in patients less than 25 years of age. Arthroscopy. 2019;35(4):1036-41.
- Pogorzelski J, Horan MP, Hussain ZB, Vap A, Fritz EM, Millett PJ: Subpectoral biceps tenodesis for treatment of isolated type II SLAP lesions in a young and active population. Arthroscopy. 2018;34(2):371-6.
- Werner BC, Lyons ML, Evans CL: Arthroscopic suprapectoral and open subpectoral biceps tenodesis: a comparison of restoration of length-tension and mechanical strength between techniques. Arthroscopy. 2015;31(4):620-7.
- Millett PJ, Sanders B, Gobezie R, Braun S, Warner JJ: Interference screw vs. suture anchor fixation for open subpectoral biceps tenodesis: does it matter? BMC Musculoskelet Disord. 2008;9:121.
- Nho SJ, Reiff SN, Verma NN, Slabaugh MA, Mazzocca AD, Romeo AA: Complications associated with subpectoral biceps tenodesis: low rates of incidence following surgery. J Shoulder Elbow Surg. 2010;19(5):764-8.
- Euler SA, Smith SD, Williams BT, Dornan GJ, Millett PJ, Wijdicks CA: Biomechanical analysis of subpectoral biceps tenodesis: effect of screw malpositioning on proximal humeral strength. Am J Sports Med. 2015;43(1):69-74.
- Beason DP, Shah JP, Duckett JW, Jost PW, Fleisig GS, Cain Jr EL: Torsional fracture of the humerus after subpectoral biceps tenodesis with an interference screw: A biomechanical cadaveric study. Clin Biomech. 2015;30(9):915-20.
- Parisien RL, Trofa DP, Kang HP, et al: Increased risk of humeral fracture with open versus arthroscopic tenodesis of the long head of the biceps brachii. Arthrosc Sports Med Rehabil. 2020;2(4):e329-32.
- Dekker TJ, Peebles LA, Preuss FR, Goldenberg BT, Dornan GJ, Provencher MT: A systematic review and meta-analysis of biceps tenodesis fixation strengths: fixation type and location are biomechanically equivalent. Arthroscopy. 2020;36(12):3081-91.