Editor’s note: This article is the second installment of a three-part series on advancements in shoulder replacement surgery. Part one, published in the June issue of AAOS Now, covered advancements in anatomical shoulder arthroplasty. Part three, published in the August-September issue, described a range of considerations in the perioperative management of patients undergoing shoulder arthroplasty.
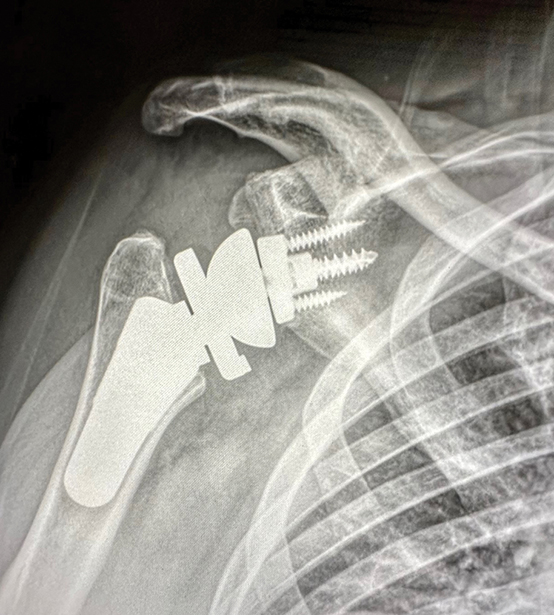
Reverse shoulder arthroplasty (RSA) has become an increasingly common option for shoulder arthropathy in the face of chronic rotator deficiency. RSA differs from traditional shoulder replacement because it shifts the center of rotation (COR) within the shoulder joint, enabling the deltoid muscle to compensate for the lack of rotator cuff function. This change in joint mechanics helps patients regain some range of motion (ROM) and function.
RSA is being performed with increasing frequency as its indications continue to expand. Indications for RSA include rotator cuff arthropathy, failed total shoulder replacement, comminuted proximal humerus fracture, and proximal humerus fracture, among others. The safety profile for RSA continues to improve as pain relief and advanced functional outcomes of the procedure have been established at long-term follow-up.
Medial versus lateral offset
Scapula notching refers to radiographic changes seen on the inferior neck and scapula pillar, presumably resulting from impingement of the humeral prosthesis on the scapula. This may lead to micromotion of the baseplate, glenoid loosening, increased polyethylene wear/osteolysis, and decreased ROM. Despite these possible issues, scapular notching has not shown a consistently negative effect on clinical outcomes; however, there are conflicting studies regarding increased complication rates when notching is present.
To minimize notching, lateralizing the COR through the glenoid, humerus, or both has become popular. This technique allows for less detensioning of the rotator cuff, which, if present, can lead to instability and weakness.
Lateralization can be achieved by bone grafting and augmentation of the glenoid, thus shifting the baseplate-glenoid interface laterally. Another option to lateralize the glenoid surface is the use of a metal augmented baseplate. Increased ROM and strength are potential advantages to a lateralized glenoid. However, increased shear forces at the baseplate/glenoid interface can occur after lateralization, potentially leading to higher rates of micromotion and loosening. In contrast to lateralization, medialization can lead to improved compressive forces at the bone/implant junction, possibly leading to improved implant stability, at the cost of radiographic notching.
Laterization of the COR can also be achieved on the humeral side of the joint. Humeral implants with a lower neck-shaft angle (NSA) were designed to help achieve a lateralized COR. As opposed to the classic Grammont-style humeral prosthesis of a 155-degree NSA, 135-degree NSA implants have become popular. These implants were also developed to decrease scapular notching and improve ROM but carry the cost of potentially higher dislocation rates. A review of the literature suggests no clear consensus on medialization versus lateralization of the glenoid.
Inlay and onlay implants
The use of inlay versus onlay designs of the proximal portion of humeral implants has been a point of debate. An inlay system increases the bony contact between the proximal humerus and implant, but the system does involve increased native-bone resection. An onlay design increases lateralization of the humerus and allows for retention of the humeral stem when converting from hemiarthroplasty to anatomic total shoulder arthroplasty or RSA. Lateralization and lengthening of the humerus can increase tension on the rotator cuff and deltoid, potentially leading to an increased rate of acromial/scapula fractures.
Multiple studies have evaluated various outcomes of RSA with a lateralized glenosphere COR and 135-degree NSA implant compared to RSA with a medialized COR and a Grammont-style, 155-degree NSA prosthesis. Although the rate of notching appears to be lower with a lateralized COR and an implant with a lower NSA degree, the difference between techniques in ROM and functional outcome scores appears to be minimal or at least inconsistent across the literature.
Screw versus post for baseplate fixation
Loosening of the glenoid component, namely the glenoid baseplate, can be a substantial complication and one of the primary modes of failure in both RSA and revision RSA. Both central post and central screw fixation with or without peripheral locking screws are common designs to help minimize this problem. Post and/or screw fixation is particularly relevant in constructs with a lateralized glenoid COR where there is more stress on the implant/glenoid interface.
Some finite element analyses suggest that screw fixation allows less micromotion than post constructs. However, complications including revision surgery, radiographic loosening, and poor clinical outcomes have been reported, and reports failed to show a significant difference between central screws and long central posts.
Jeffrey Berg, MD, FAAOS, is a shoulder and sports medicine specialist who practices at Town Center Orthopaedics in Reston, Va.
Aaron Carter, MD, FAAOS, is a shoulder and knee specialist who practices at Town Center Orthopaedics in Reston, Va.
Thomas Fleeter, MD, MBA, FAAOS, is in private practice in Reston, Va., with Town Center Orthopaedics. He is also a member of the AAOS Now Editorial Board and chair of the AAOS Committee on Professionalism.
Ryan Miyamoto, MD, FAAOS, is a shoulder and sports medicine specialist at Town Center Orthopaedics in Fairfax, Va.
References
- Bercik MJ, Werner BC, Sears BW, et al: A comparison of central screw versus post for glenoid baseplate fixation in reverse shoulder arthroplasty using a lateralized glenoid design. J Clin Med 2022;11(13):3763.
- Torkan LF, Bryant JT, Bicknell RT, Ploeg HL: Central fixation element type and length affect glenoid baseplate micromotion in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2022;31(7):1385-92.
- Harmsen SM, Robaina J, Campbell D, Denard PJ, Gobezie R, Lederman ES: Does lateralizing the glenosphere center of rotation by 4 mm decrease scapular notching in reverse shoulder arthroplasty with a 135° humeral component? JSES Int 2022;6(3):442-6.
- Freislederer F, Toft F, Audigé L, et al: Lateralized vs. classic Grammont-style reverse shoulder arthroplasty for cuff deficiency Hamada stage 1-3: does the design make a difference? J Shoulder Elbow Surg 2022;31(2):341-51.